Ideelt sett er det best å velge en test som både er svært spesifikk og svært sensitiv når man tester for en sykdom. I praksis er en test med høy sensitivitet god til å finne dyr med sykdommen og vil derfor gi få falske negative resultater. En test med høy spesifisitet gir et positivt resultat hos dyr som virkelig har sykdommen, og vil derfor gi få falske positiver.
Men ingen av testene for Cushings har både høy følsomhet og høy spesifisitet – alle er et kompromiss mellom de to. Dette betyr at de diagnostiske testene vi har for hyperkortisolisme hos hunder ofte må brukes i kombinasjon for å være sikre på diagnosen.
(Merk: Prosentverdiene som er oppgitt for sensitivitet og spesifisitet nedenfor, skal betraktes som omtrentlige og er representative for flere undersøkelser om dette emnet. Forfatteren henviser leseren til 2019 Bennaim et al review for ytterligere informasjon).
ACTH stimuleringstest (ACTHST):
Høy spesifisitet (90 %), moderat sensitivitet (85 % PDH og 50 % ADH)
Falske positive er mindre vanlig. Falske negative er ganske vanlig.
Suppresjonstest med lavdose deksametason (LDDST):
Moderat spesifisitet (70 %), høy sensitivitet (95 %).
Falske positive er ganske vanlig. Falske negative er mindre vanlige.
Urinkortisol: Kreatinin-ratio (UCCR):
Dårlig spesifisitet (20 %), høy sensitivitet (97 %).
Falske positive er vanlig. Falske negative er mindre vanlige.
Når du tolker noen av disse testene, er det verdt å vurdere den positive og negative prediktive verdien. Positiv prediktiv verdi (PPV) er andelen av hunder med en positiv test som virkelig har Cushings. Negativ prediktiv verdi (NPV) er andelen av hunder med en negativ test som ikke har sykdommen.
De positive og negative prediktive verdiene tar både testen og populasjonen som testes med i beregningen. Hvis du bruker en test i to populasjoner med forskjellig sykdomsprevalens, vil de prediktive verdiene være forskjellige. Derfor varierer PPV og NPV avhengig av hvor ofte du tester.
Når du tolker noen av disse testene, er det verdt å vurdere den positive og negative prediktive verdien. Positiv prediktiv verdi (PPV) er andelen av hunder med en positiv test som virkelig har Cushings. Negativ prediktiv verdi (NPV) er andelen av hunder med en negativ test som ikke har sykdommen.
De positive og negative prediktive verdiene tar både testen og populasjonen som testes med i beregningen. Hvis du bruker en test i to populasjoner med forskjellig sykdomsprevalens, vil de prediktive verdiene være forskjellige. Derfor varierer PPV og NPV avhengig av hvor ofte du tester.
Hvis vi skulle teste nesten alle pasienter vi ser (en populasjon med lav prevalens – 5 %)
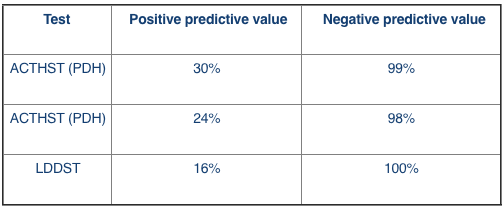
I dette scenarioet, hvis vi bruker LDDST, kan vi være 100 % sikre på at et negativt resultat virkelig er negativt. Mens bare 16 % av de positive resultatene vil faktisk ha Cushings.
- Hvis vi var mer kritiske til pasientene vi tester vi (en populasjon med høy forekomst – 90 %)
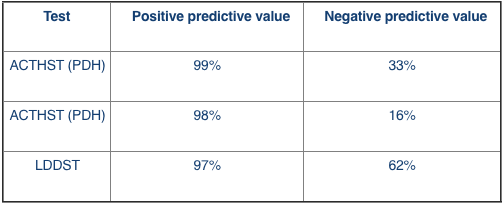
I dette scenarioet, hvis vi bruker LDDST, vil 62 % av de negative resultatene virkelig være negative og 97 % av de positive resultatene vil ha Cushings.
Konklusjon
ACVIM Consensus Statement panel 2012 (Behrend et al. 2013) regnes som en lavdose deksametason-suppresjonstest (LDDST) som den foretrukne screeningtesten med mindre det er mistanke om iatrogen Cushings. På grunn av den lavere følsomheten til ACTH-stimuleringstesten er den diagnostiske nytten som screeningtest dårligere ved naturlig forekommende Cushings syndrom enn LDDST.
Det er imidlertid også viktig å ta hensyn til andre faktorer ved valg av diagnostisk test, inkludert testtilgjengelighet, kostnader og samtidig sykdom hos pasienten. Og like viktig er det å forbedre det potensielle utfallet av testen ved å sikre en høy grad av mistanke om sykdom før det gjennomføres bekreftende testing.



